| World Journal of Nephrology and Urology, ISSN 1927-1239 print, 1927-1247 online, Open Access |
| Article copyright, the authors; Journal compilation copyright, World J Nephrol Urol and Elmer Press Inc |
| Journal website http://www.wjnu.org |
Case Report
Volume 3, Number 1, March 2014, pages 63-65
High-Grade Primary Leiomyosarcoma of the Kidney
Hakan Ozturka, c, Serap Karaaslanb
aDepartment of Urology, School of Medicine, Sifa University, Izmir, Turkey
bDepartment of Pathology, School of Medicine, Sifa University, Izmir, Turkey
cCorresponding author: Hakan Ozturk, Basmane Hospital of Sifa University, Fevzipasa Boulevard No: 172/2, 35240, Basmane-Konak-Izmir, Turkey
Manuscript accepted for publication March 24, 2014
Short title: Leiomyosarcoma of the Kidney
doi: https://doi.org/10.14740/wjnu158e
| Abstract | ▴Top |
Leiomyosarcomas account for 0.8 to 2.7% of all malignant renal tumors. Like the leiomyomas, the leiomyosarcomas originate from the cells of the renal capsule, pelvis renalis, the calyces and smooth muscle of the blood vessels. They are two-folds more common in women and most frequently seen in the fourth and sixth decades. They are solitary lesions. Their major symptoms are pain, palpable mass and hematuria. Clinical, radiological and pathological findings of a 51 years old patient presenting with diagnosed flank pain and nausea and diagnosed as having high-grade primary renal leiomyosarcomas were evaluated under the light of current literature.
Keywords: Leiomyosarcoma; Kidney leiomyosarcoma; Sarcoma; Radical nephrectomy
| Introduction | ▴Top |
Leiomyosarcomas are malignant aggressive tumors with high potential of metastasis usually originating from the soft tissues and smooth muscle of the uterus. Renal leiomyosarcoma may originate from the renal pelvis, calyces, renal capsule and renal vessels but their most common site of origin is smooth muscle of the renal veins [1]. Fifty to sixty per cent of the renal sarcomas are leiomyosarcoma. It is very difficult to differentiate them from other renal masses prior to operation [2]. Among the urogenital sarcomas, the renal leiomyosarcomas are less common compared to prostatic or bladder sarcomas but they show a more fatal prognosis. Renal leiomyosarcomas reach big sizes. The reason for this is their mesenchymal components and they are devoid of natural barriers like those in other types of tumor. The sarcomas have typically pseudocapsule.
| Case Report | ▴Top |
A 51 years old man presented with flank pain and nausea being present over the last 4 months. The biochemical analyses were as follows: AST and ALT normal, FBG: 123 mg/dL; TSH: 0.713 mIU/mL, creatinine: 0.75 mg/dL, urea 26 mg/dL, hemoglobin 13.3 g/dL, WBC: 4,100/mm3, hematocrit: 38.7%, platelets: 230,000/mm3. Physical examination was unremarkable. Medical history of the patient revealed hypertension, diabetes mellitus and hypothyroidism. Renal ultrasound (US) examination revealed hyperechogenic solid mass which was 70 × 58 × 66 mm in size on the left renal pelvis. On MRI examination, grade II hydronephrosis was found on the left kidney and a mass lesion of 78 × 58 × 68 mm was found on the renal hilus which was hypointense on the T1-weighted images and hyperintense on the T2-weighted images and invading the renal pelvis (Fig. 1, 2). Apparent contrast enhancement was observed. The surrenal gland was normal in appearance. There was no lymph node on the para-aortic area. The patient underwent left transperitoneal radical nephrectomy.
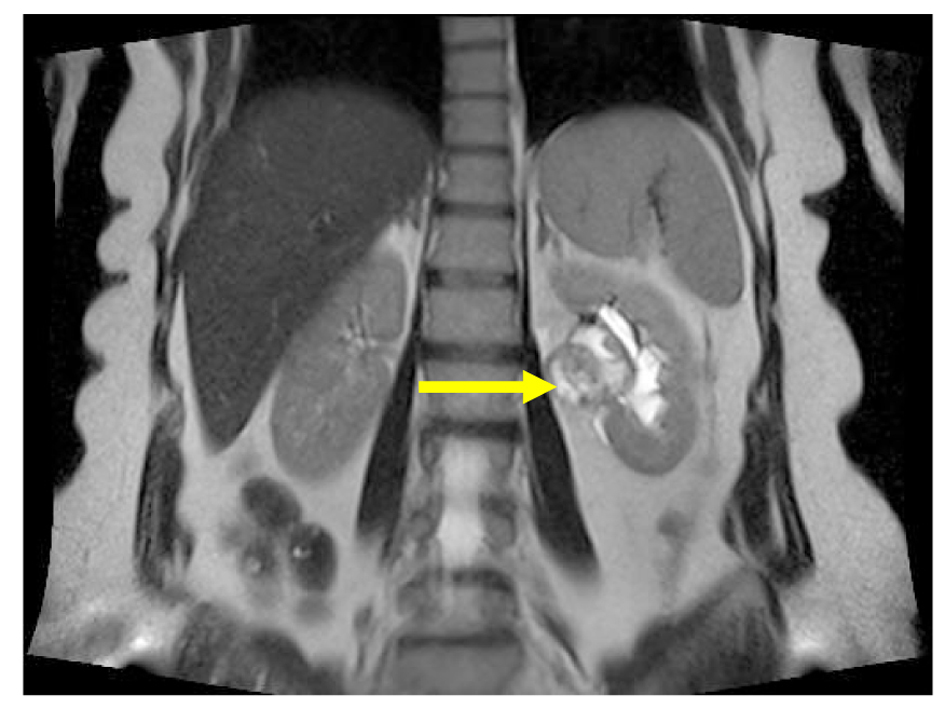 Click for large image | Figure 1. Magnetic resonance imaging: mass in pelvis renalis of left kidney (arrow), the coronal reconstruction shows. |
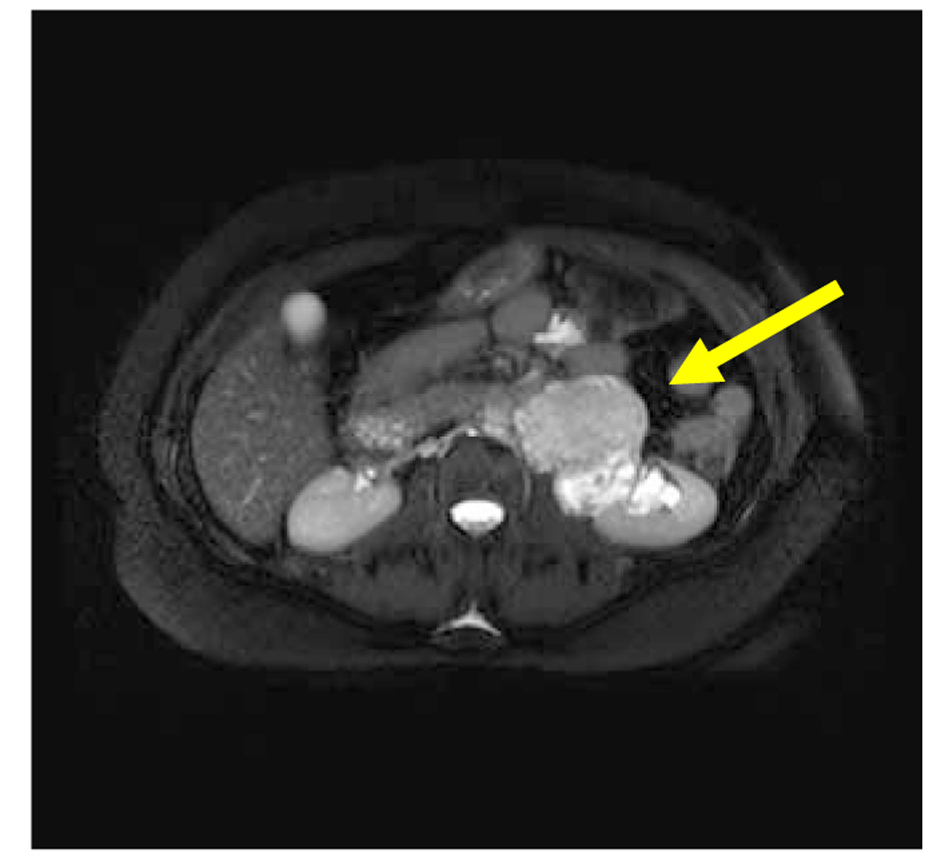 Click for large image | Figure 2. Magnetic resonance imaging: mass in pelvis renalis of left kidney (arrow), the axial shows. |
Pathological examination revealed primary high-grade renal leiomyosarcoma. Macroscopic findings were as follows: A tumor with the biggest diameter of 8 cm was seen on the renal hilus which was pinky-yellow in color, well-circumscribed and showing hemorrhages and cystic features in a focal area (Fig. 3). Microscopic examination reported that pleomorphism (small picture) and necrosis (blue arrow) were remarkable in the tumor consisting of the cells with pink cytoplasm and spindle nucleus crossing with each other from several angles. Rates of necrosis and mitosis were 16-20/10HPF (Fig. 4) (H&E, × 100, 200). In the immunohistochemical examination DKA was positive, desmin (+), CD117 (-), CD34 (-) and S-100 was (-) (Fig. 5, 6). Ki-67 proliferation index was found to be 15%. No distant metastases were found on the PET/CT. The patient was placed in follow-up program.
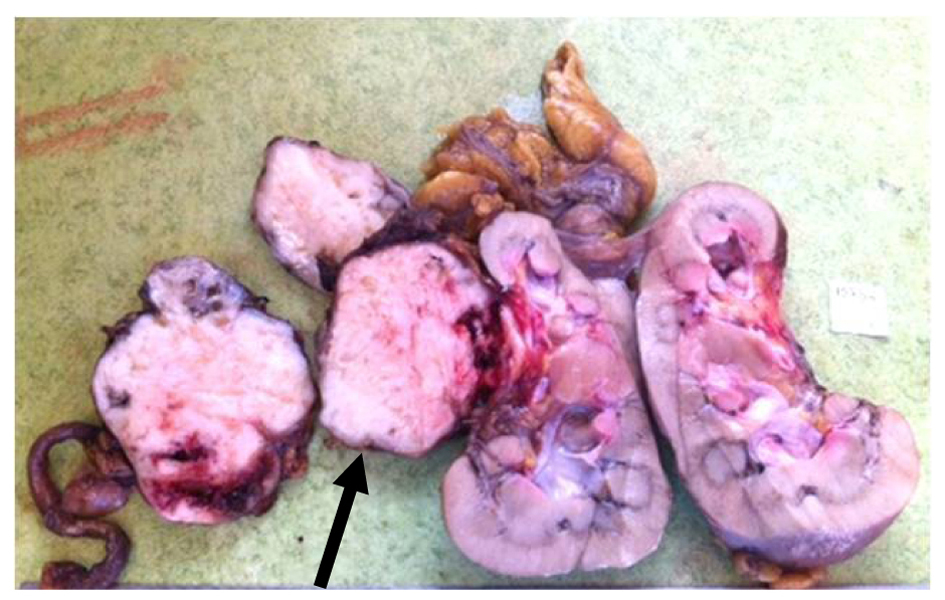 Click for large image | Figure 3. Surgical specimen. Tumor in pelvis renalis of left renal kidney (arrow). |
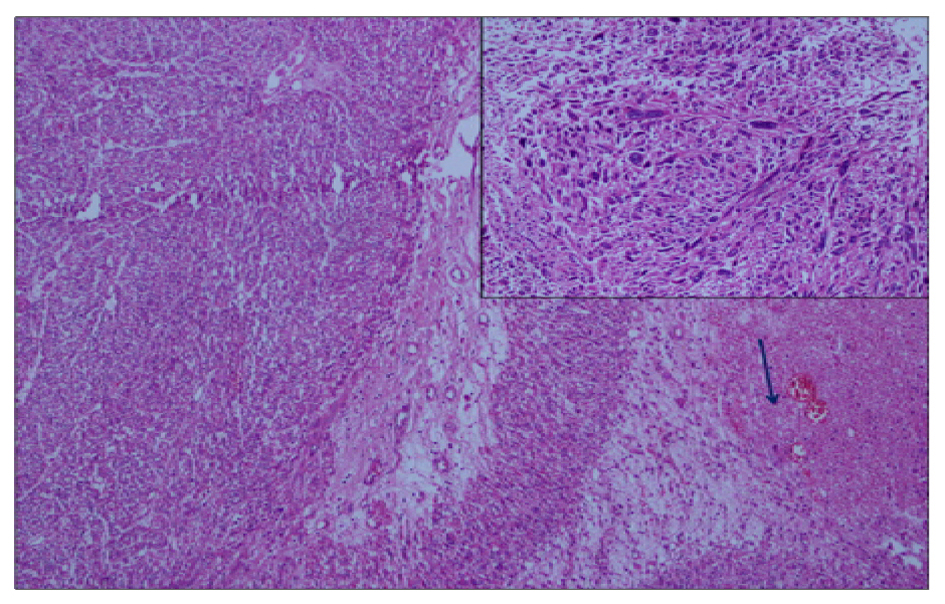 Click for large image | Figure 4. Hematoxilyn-eosin staining demonstrating high-grade sarcomatoid cells. H&E (× 100, 200). Pleomorfism (small figure) and necrosis (arrow). |
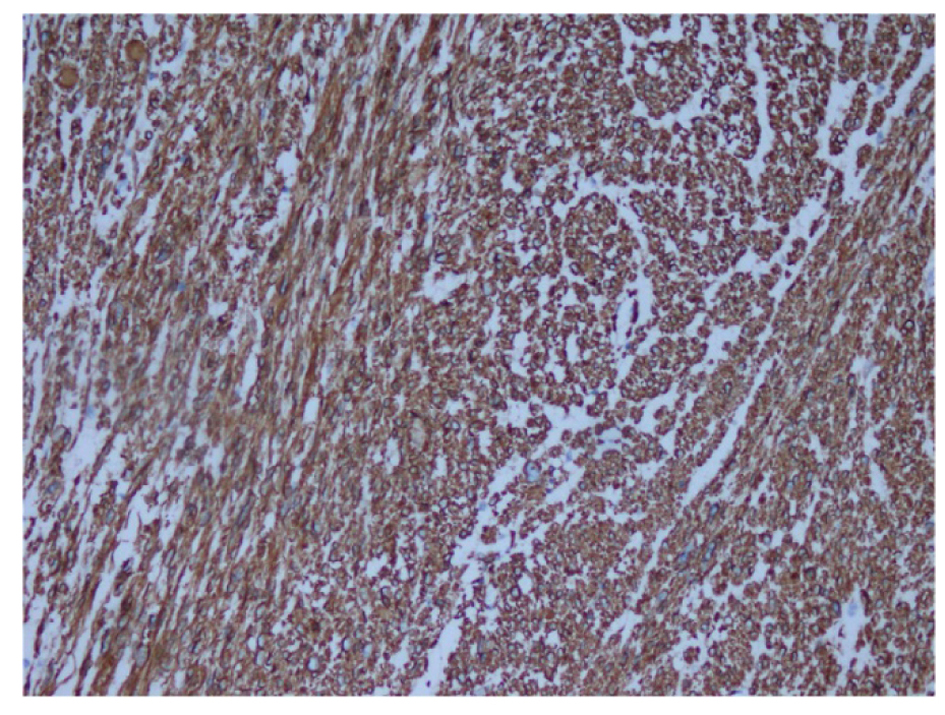 Click for large image | Figure 5. Immunohistochemistry showing diffuse actin expression in smooth muscle fiber cytoplasm. Actin (× 200). |
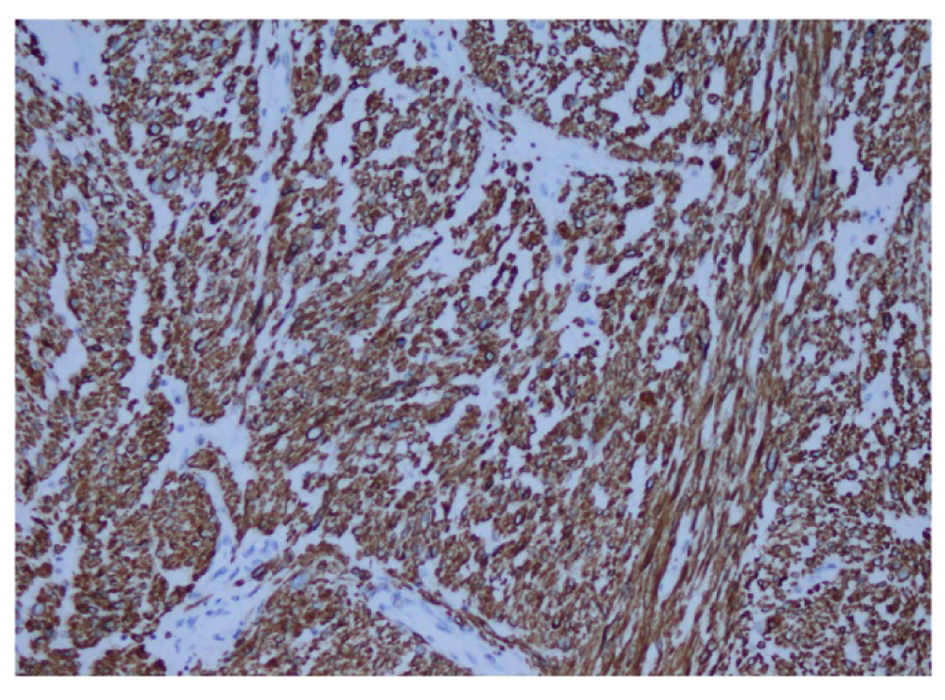 Click for large image | Figure 6. Immunohistochemistry showing desmin (× 200). |
| Discussion | ▴Top |
Differentiating the renal leiomyosarcoma from the renal cell cancer showing sarcomatoid differentiation is very difficult because they have similar clinical, radiological and pathological features. Clinically, lumbar or abdominal mass reaching to palpable size, pain in the lumbar or abdominal area and rarely hematuria are seen. They may reach big size. The most important features of the sarcomas differentiating them from the renal cell carcinomas are that they originate from the capsule of perisinusoidal region, they can reach big size without lymphadenopathy and they have components appearing as liposarcomas and osteosarcomas in the lesion. They are avascular except for the subtype of hemangioperistom. Sarcomas should be considered in the situation of rapidly growing renal masses. Sarcomas have pseudocapsule but this is a surgically unreliable barrier because it is usually infiltrated by the tumor. High-grade sarcomas are usually tumors with high potential for metastasis. The most common site of metastasis is the lungs. The liver and lymph nodes are the second most common site of metastasis [1]. Low-grade sarcomas frequently cause local recurrences and surgical removal of the recurrence extends the survival.
Pathological feature of the leiomyosarcomas is spindle cells with wide eosinophilic cytoplasm. Cellular pleomorphism, multinuclear giant tumor cells and coagulation necrosis in the tumor cells are remarkable. Many histological subtypes other than leiomyosarcomas have been defined for the renal sarcomas, including liposarcoma, osteogenic sarcoma, rhabdomyosarcoma, fibrosacrcoma, carcinosarcoma, malignant fibrotic histiocytoma, angiosarcoma and malignant hemangioperistoma. Epitheloid angiomyolipoma, a variant of angiomyolipoma, and sarcomatoid renal cell carcinoma are the tumors most frequently confused pathologically with leiomyosarcoma. They are differentiated with immunohistochemical staining with smooth muscular actin and desmin [3]. Generally, the most important prognostic feature in the sarcomas is presence of tumor on the surgical margin and grade of the tumor. Radical nephrectomy is the primary therapeutic method for the renal leiomyosarcoma [4].
Nonetheless, chemotherapy and radiation therapy are recommended if the surgical margin is positive and in the presence of metastatic disease. The renal leiomyosarcomas have high potential for local recurrence and metastasis. Because of this, 5-year survival rate is about 29-36%. Most patients die within 1 year after time of diagnosis because of poor prognosis [5]. No therapeutic protocol has been defined for adjuvant chemotherapy but sunitinib, a tyrosine kinase inhibitor, has been shown to be beneficial in the phase-II studies [6].
Conclusion
Primary leiomyosarcoma of the kidney is a rare tumor but acts very aggressively with high potential for metastasis. The patients should be followed closely. High-grade renal leiomyosarcoma should be treated with a multidisciplinary approach including sufficient surgical excision, radiation therapy and adjuvant chemotherapy.
| References | ▴Top |
- Venkatesh K, Lamba Saini M, Niveditha SR, Krishnagiri C, Babu S. Primary leiomyosarcoma of the kidney. Patholog Res Int. 2010;2010:652398.
- Martinez-Cornelio A, Ramos-Salgado F, Hernandez-Ramirez D, Garcia-Alvarez KG, Alvarado-Cabrero I, Hernandez-Toriz N. Leiomyosarcoma of the kidney: case report. Cir Cir. 2011;79(3):260-263, 282.
- Mai KT, Perkins DG, Collins JP. Epithelioid cell variant of renal angiomyolipoma. Histopathology. 1996;28(3):277-280.
doi pubmed - Demir A, Yazici CM, Eren F, Turkeri L. Case report: good prognosis in leiomyosarcoma of the kidney. Int Urol Nephrol. 2007;39(1):7-10.
doi pubmed - Dominici A, Mondaini N, Nesi G, Travaglini F, Di Cello V, Rizzo M. Cystic leiomyosarcoma of the kidney: an unusual clinical presentation. Urol Int. 2000;65(4):229-231.
doi pubmed - Mahmood ST, Agresta S, Vigil CE, Zhao X, Han G, D'Amato G, Calitri CE, et al. Phase II study of sunitinib malate, a multitargeted tyrosine kinase inhibitor in patients with relapsed or refractory soft tissue sarcomas. Focus on three prevalent histologies: leiomyosarcoma, liposarcoma and malignant fibrous histiocytoma. Int J Cancer. 2011;129(8):1963-1969.
doi pubmed
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
World Journal of Nephrology and Urology is published by Elmer Press Inc.